Plantar plate injuries are easily missed and probably under diagnosed here in the UK. I think part of the reason for this is a lot of people don’t know what the plantar plate is. It comes back to the old saying, if you are not looking for it, you will never find it! Quite often it is grouped together with the term metatarsalgia, however this it not a diagnoses, rather just a description for pain in the ball of the foot. So what is the plantar plate?
The plantar plate is a deep fibrocartilaginous structure which originates from metatarsal head and attaches to the proximal phalanx through the joint capsule within the forefoot. Its role is to help stabilize the metatarsophalangeal joints (MTPJ), along with a couple of other structures. The plantar plate also acts as an attachment site for the plantar fascia, so if you load the foot, the medial arch lengthens, the plantar fascia tightens, this engages the plantar plate to plantar flex the proximal phalanx, until the toe reaches the ground. This is a simplification of a complex process and is commonly known as the reverse windlass mechanism.
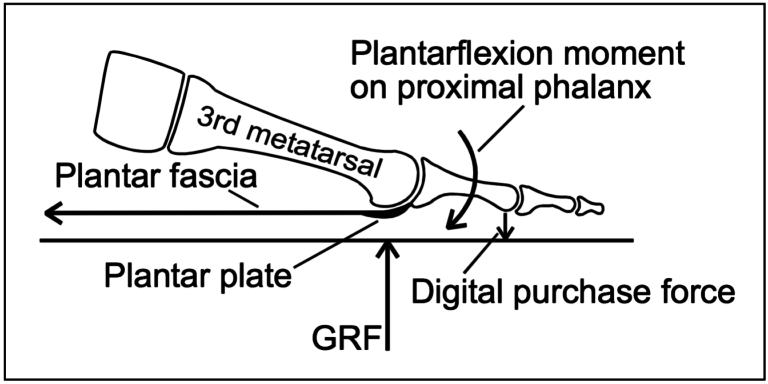
Stainsby4 described a simple yet effective way in testing the reverse windlass mechanism called the ‘footstool edge test’ (Fig 2) which involves standing on the edge of a stool at the MTPJ level and allowing the digits to hang over the edge. In a positive reverse windlass the proximal phalanges go into plantar flexion. If the proximal phalanges are in the same position on the ‘footstool edge test’ as to relaxed stance, this shows a non-functioning reverse windlass mechanism, which could be indicative of a plantar plate rupture.
Plantar plate injury may be one of the most common causes of second MTPJ pain.5 The increase in the number of plantar plate tears and ruptures being diagnosed is thought to be due to advances in imaging.6,7 There are many contributing factors. The first is any activity that expose the MTPJ to repetitive and excessive dorsiflexion (resulting in increased metatarsal GRF), so think about jumping and running and, in clinic, I tend to see more of these plantar plate injuries in forefoot runners.
There are a few biomechanical causes that will increase the load through the plantar plate including hallux valgus (bunions), as the function through the 1st MTPJ is reduced, then we get what is known as low gear propulsion and increase loading through lesser MTPJs, typically the 2nd, 1st, then 3rd and so on. Also having an irregular metatarsal length, for example if you have a long 3rd metatarsal, can expose the plantar plate to increased load, as can external factors like high heels.
Same style of test to assess ACL tears, helps to assess integrity of the plantar pate, it is quick, easy and a simple test to perform. Stabilise the head of the metatarsal with one hand, using the other hand stabilise the base of the proximal phalanx, apply a vertical force, we are looking for pain and any translocation, it is important to remember this is different from dorsiflexion of the digit.
One study showed sensitivity of 80.6% (positive vertical stress test with tear identified intraoperatively) and a specificity of 99.8% (negative vertical stress test with intact plantar plate intraoperatively)

Orthoses, can be a useful way to help offload the affected plantar plate, using a metatarsal dome just proximal to the affected metatarsal head and then a sulci extension with a cut out around the MTPJ region (Fig 7). Combining the orthoses, taping and footwear advice can be quite an effective way of offloading the affected plantar plate, whilst the patient reduces sporting activities.
Steroid injection – A staggered course of steroid injections reaching a maximum of once ever 1 to 3 months and a maximum 3 in a 12 month period has been shown to effective and safe, however repeated intra-articular injections has been shown to result in dislocation of the MTPJ.12,14,15 it has also been suggested that injections into a ligament resulted in destruction of fibrocytes and reduction in tensile strength for up to 1 year16 which in turn may result in further damage a possible rupture.
A recent case study showing a patient with a plantar plate tear, was managed using conservative measures, consisting of taping, activity modification and the use of a Darco boot over a 6 month period, and progressing to stiffed shoe and orthoses (however the orthoses where not described) and stopped taping. At the 1 year mark, the patient was pain free with no toe deformity, and on MRI the plantar plate has healed.